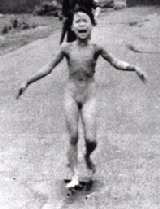
A University of Minnesota medical student goes to Vietnam to discover his heritage and learn about caring for the poor.
By Gail Rosenblum
HANOI, Vietnam —It’s 8 a.m. at the National Institute of Pediatrics in Hanoi. The finest children’s hospital in Vietnam, it has no elevator and all of the medical manuals are photocopied.
Sixteen men in white coats sit in castoff mustard-yellow chairs and discuss the morning’s cases. A nurse brings tea in a cheerful flowered carafe, pours it into 10 stained glasses, and sets the carafe next to an ashtray stuffed with cigarette butts.
The doctors have been joined this morning by two American visitors.
Phuong Nguyen, a 24-year-old medical student from the University of Minnesota class of 2004, has been at the hospital for two weeks, observing and assisting in surgery. For two weeks prior, he lived in a small province to the north, joining a group of volunteer physicians fixing cleft lips and palates. Born in a refugee camp in Indonesia in 1979 as his educated, middle-class parents fled the communist takeover of Vietnam, and raised across the world in Maplewood, Minnesota, Phuong had never seen his parents’ home country. His desire to do so was keen.
In his third year of medical school in 2003, he learned about a humanitarian medical program sponsored by the American Academy of Pediatrics called Project Vietnam. For the young man raised in privilege, this was the perfect avenue for return. “To have come back solely as a tourist would have felt empty,” he says.
But Phuong’s 57-year-old mother, Mai, who stands at his side, cherished the opportunity to return as a tourist—to visit distant cousins, shop, and sun on the beaches—after her harrowing escape 25 years ago. Still, she smiles as she confesses to another agenda. “I come to make sure he doesn’t get married off,” she says with a laugh. Out of earshot, her voice turns serious. “He’s a young man who is living in America, raised in America. He’s very honest, not knowing any tricks behind the scenes. Here, people will try to take advantage. He says, ‘Don’t worry, Mom.’ But, as a mom, I still worry.”
Phuong introduces Mai to the group and takes his place in a seat across the room. There will be 11 surgeries today, including one on a 2-month-old boy with a brain hemorrhage and another on a 14-year-old girl with a cerebral tumor. Most of the children’s parents are shopkeepers and farmers. Nearly all are destitute. No one has medical insurance, so they must pay out of pocket. Many have had to carry their children on buses or strap them onto bicycles. Some travel as far as 100 miles to get to the tertiary-care hospital; others come from nearby villages approximately 20 miles away.
Lessons Not Taught in Class
To get the most out of their limited resources, the surgeons have learned tricks they would never find in a medical manual, photocopied or otherwise. A single suture costs 40,000 dong, or $2.80 in U.S. dollars, seemingly a pittance. But the annual income of a Vietnamese family averages $270. To compensate, these doctors are among the most skilled in the world at closing a wound in two or three tidy stitches instead of eight or 10.
If a family arrives in clean clothes, signaling relative affluence, the doctors hike the price of care from perhaps $30 to $300. They then save the extra money and use it to cover expenses for the next family, who will undoubtedly arrive with no way to pay.
Phuong suggests that his mother wait for him outside the operating room. She wants to stay. OK, he agrees, telling her not to touch anything because all the equipment has been sterilized.
“I know that,” she says, rolling her eyes and flipping her hand in the direction of her son. Mai, who earned a biochemistry degree in 1972 in Saigon (now Ho Chi Minh City, 700 miles south of Hanoi), scrubs and stands near the wall. She, too, wanted to be a doctor, but the rigors of study intimidated her. When Phuong was 2, she bought him a toy medical kit. When her son struggled with biology in high school, she taught him tricks for memorizing Latin words until he was “the top of his class.”
Phuong graduated from the University of Minnesota in two years with a degree in neuroscience, spent one year doing research at Harvard University, and began medical school in 2000.
For Phuong the main attraction of coming to Vietnam was the promise by doctors who had participated in Project Vietnam that he would see things here that he wouldn’t see during an entire two-year fellowship in the United States. He hasn’t been disappointed. In one afternoon, for example, he saw a choledochal cyst, imperforate anus, two cases of patent ductus arteriosis, two children with ventricular septal defect, one child with syndactyly, an anovaginal fistula, two teratomas, and much more. Some of those conditions would never be seen in the United States.
Through the Eyes of an American
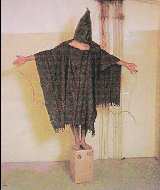
The operating room is a study in contrasts. The overhead light and LCD monitors are state of the art, but the scissors are dull and missing tips. The sheets on which children lay, the plastic gloves, and all of the instruments will be washed and reused. Surgeons use sutures made of cotton as opposed to silk, nylon, or absorbent materials.
These little things weigh heavily on Phuong’s conscience. Until coming here, he never considered the “enormous waste” of materials used in surgery. “We use dozens of sutures, throw away towels, so many things,” he says.
Suddenly, surgery stops. The power has gone out. “Merde!” the lead surgeon curses in French. Seconds later, the power returns. The team continues. Power will go out another six times before the surgery is completed. Blackouts are common in Vietnamese hospitals, where back-up generators are at least 20 years old and often unreliable.
Pediatric surgeon Nguyen Thanh Cong, M.D., who trained in Japan, was performing heart surgery on an infant in the room next to Phuong’s when the power went out. Asked later about this particularly troublesome challenge, he answered simply: “Vietnam is a poor country.”
And, with that, the conversation ended.
Outside surgery, the narrow hallways are lined with anxious parents dressed in blue and brown striped hospital pajamas that resemble jail uniforms. Some sleep on the floor, others pull from bags miniature bananas and baguettes —the latter a reminder of decades of French colonial rule. One sallow-cheeked father sits on a flattened cookie box. A woman screams at a man as both push frail children down the hall. She thinks he has stolen her baby’s blanket. Her howls fill the hallway until another man steps in and demands that she stop.
When their children get through postop, parents maneuver them on rolling metal stretchers lined with straw mats to recovery rooms with eight or 10 beds. Sometimes two children share a bed.
Phuong, in his white coat, and Mai, clutching her purse, step into a recovery room where a mother nurses her 2-year-old son, who is dressed in Harry Potter pajamas.
Phuong and Mai have vaulted to near celebrity status as they walk from recovery room to room. Parents look up in hope of having a conversation with the unusual Vietnamese speakers with their lighter skin and rosy cheeks. (Visitors such as these two are known as “Viet Kieu,” an uncomplimentary term for the ones who left.)
Phuong delights his mother as he passes out toys and bite-size chocolates to the children. “This morning I tell Phuong to bring candy,” Mai says. “He say, ‘Mom, you are goofy.’ But look at this! Now they are happy.”
Amid the poverty, mother and son are moved by the effortless nurturing they see everywhere they look. Parents never leave their children’s sides, lying with them, stroking their hair and skin, cooing to them. Before coming here, Phuong spent two weeks in Hoa Binh, a province in northern Vietnam, with Project Vietnam. There, the group of surgeons Phuong worked with performed 18 cleft lip and palate surgeries but had to turn down dozens more patients when resources ran out. That still haunts the handsome young medical student, as many of the patients were teenagers only a few years younger than he with holes in their upper lips that caused food to ooze out. “Please fix this,” their parents begged. “Otherwise, our child has no chance to marry.”
During his time in Hoa Binh, Phuong translated for one American doctor and served as a scrub nurse for others. Team members brought their own anesthesia medications, ambu bags, and surgical instruments. Because of the hospital’s antiquated power supply, there often was insufficient light to do the surgeries, so Phuong would wear a Halogen headlamp he purchased at REI on his forehead. One doctor, absent a ventilator, squeezed a hand-held balloon for 10 straight hours during surgery. After surgery, Phuong carried the children up a flight of stairs to recovery.
Not surprisingly, Phuong feels a universe away from his $80,000 U.S. medical school education. “My hands aren’t exactly calloused from manual labor,” he says, humbled by having grown up in such affluence and seeing how different his life would have been had his family decided to stay in Vietnam.
Phuong’s plans after graduation were to begin a five-year residency in general surgery at New York University Medical Center. But his Vietnam experience has already had a lasting impact. “I’d really like to come back and contribute something,” he says. “I feel a responsibility to make good.”
Mai is deeply proud of her son—and of his desire to one day return to his home country and make a difference. “As I’m watching him, I’m thinking about a little kid running around on an [Indonesian] island, and he grew up and he’s a doctor… And he’s right. He needs to contribute to Vietnam. It’s his country.” MM
Gail Rosenblum is a Minneapolis writer. She and photographer Judy Griesedieck traveled to Vietnam in April as part of a four-year project on the University of Minnesota Medical School class of 2004. Other stories about the class of 2004 have been published in the Minneapolis Star Tribune.
Giving Kids a Chance
Project Vietnam, the international health program of the American Academy of Pediatrics, was founded in 1996 by California pediatrician Quynh Kieu, M.D., and her husband, anesthesiologist Chan Kieu. When the United States resumed diplomatic relations with Vietnam that year, the Kieus returned to their home country in the hope of improving the dismal state of health many Vietnamese children suffered.
By 1998, they were making regular trips to Vietnam with fellow volunteers to perform surgeries on children with cleft lips, cleft palates, and strabismus. In 2000, they added cataract surgeries and ear exams to Project Vietnam’s offerings.
Among the biggest threats to children in Vietnam’s provinces, as well as in larger cities including Hanoi, is brain hemorrhage caused by a lack of Vitamin K. A study of Vietnamese children by the National Institute of Pediatrics in 2000 found that they had a deficiency rate that was 20 times higher than the rate in developed countries. They also had the highest deficiency rate in Asia. Of 1,325 infants hospitalized in Hanoi between 1991 and 1998, more than 17 percent died and 40 percent showed long-term damage from lack of Vitamin K.
With Project Vietnam’s support, the institute launched demonstration projects in two districts with the highest incidence of Vitamin K deficiency hemorrhage, Ha Tay and Hanoi. With the support of AmeriCares, VNHELP, the Vietnamese Pharmacists Association, International Children Assistance Network, and Lua Viet, some 120,000 doses of Vitamin K have been donated to the program, and about 25,000 babies in the two districts have received injections. Last year, the Ministry of Health adopted administration of Vitamin K for newborns as a national policy. The vitamin is currently being given to newborns in some communal health centers.
In addition, Project Vietnam leads programs to carry out nutrition assessments of children at elementary schools. Volunteers tell wrenching stories of children complaining of stomachaches when, in reality, they were simply hungry. More than 90 percent of the children studied did not get milk and were, not surprisingly, at the low end for growth. In addition, some children ate just once a day. To this end, Project Vietnam has begun a school-based project to provide nutrition support to poor families. —G.R.
For more information on Project Vietnam go to www.projectvietnam.net or write Project Vietnam, 12377 Lewis Street, Suite 103,Garden Grove, CA 92840; phone 714/641-0850.
Facts on Health Care in Vietnam
The health care system in Vietnam is a four-tier system, with 826 state-owned hospitals (central, provincial, and district), including 29 central facilities such as the National Institute of Pediatrics in Hanoi. The fourth tier is made up of five private hospitals and two foreign-owned hospitals. The country also has 19,500 private clinics and medical centers, and 10,165 communal health centers that serve collective communities of up to 10,000 people. National preventive programs such as immunization, maternal and child care, safe water, maleria prevention, family planning, and HIV prevention are managed at the central level.
Since reforms began in 1987, Vietnam has successfully achieved steady economic growth, resulting in a rapid reduction in poverty. The most recent figures on living standards show that the ratio of absolute poor has dropped from 51 percent of the population to around 35 percent in 1998. Despite strides in economic progress, the rural health sector has remained stagnant. Under the old central-planning system, social services were free, and the state was the sole provider and funder of care. Under the new system, user fees were introduced and private providers allowed to operate. People living in urban areas rely on social insurance and social welfare, while the rural social protection system depends largely on family support and informal mechanisms combined with public poverty alleviation programs. Increasingly, people living in rural areas have to shoulder a large portion of the costs of health services as user fees have increased steadily. Vietnam still feels uneasy about private sector involvement in the delivery of health services.
According to the latest health care statistics released by the Ministry of Health in 2003, each person in Vietnam spends an average of 217,300 dong annually ($14) on check-ups and treatment. Each person falls ill 1.5 times a year, and people of working age take an average of 5.8 days of leave every year for health reasons.
Among children under age 5, 30 percent suffer from malnutrition and 1.3 percent from obesity. Nearly 80 percent of the obese children live in urban areas. Monthly per capita income of Vietnamese people was 357,000 dong ($23) in 2001-2002.
Health care training is carried out in eight medical and pharmaceutical schools and 25 secondary schools and produces approximately 2,000 graduates annually. Training and management concepts are outdated, and there are few in-service training sessions. A physician earns about $35 a month; a nurse, $32, in urban areas.
This year, the government started an initiative to implement national health insurance. However, the system differs from province to province. Ha Nam province, for example, chose to provide matching funds to purchase coverage for more than 90,000 indigent residents, giving them access to health care facilities of their choice, while Lang Son set aside government funding to reimburse for health services as incurred. Nonetheless, this is a crucial step to shore up the safety net and reverse disturbing trends evident in the country’s health sector.
Reprinted from an article published by the Minnesota Medical Association:
file:///c:/windows/Temporary%20Internet%20Files/OLKA2E1/Rosenblum.htm[Thank you, Fongue!]